THE NATION DEBATE ON HEALTHCARE in the United States — which has been going on for decades — centers on who should be covered and who should pay the bill. It’s an argument that has no clear answers and cannot be easily resolved because of two fundamental realities: Health care is expensive, and Americans are sick.
Americans benefit from highly trained personnel, remarkable facilities and access to the newest drugs and technologies. Unless we eliminate some of these benefits, our health care will remain costly. We can trim around the edges — for example, with changes in drug pricing, lower administrative costs, reductions in payments to hospitals and providers, and fewer defensive and unnecessary procedures. These actions may slow the rise in health care spending, but costs will keep rising as the population ages and technology advances.
And Americans are sick — much sicker than many realize. More than 100 million adults — almost half the entire adult population — have pre-diabetes or diabetes. Cardiovascular disease afflicts about 122 million people and causes roughly 840,000 deaths each year, or about 2,300 deaths each day. Three in four adults are overweight or obese. More Americans are sick, in other words, than are healthy.
Instead of debating who should pay for all this, no one is asking the far more simple and imperative question: What is making us so sick, and how can we reverse this so we need less health care? The answer is staring us in the face, on average three times a day: our food.
Poor diet is the leading cause of mortality in the United States, causing more than half a million deaths per year. Just 10 dietary factors are estimated to cause nearly 1,000 deaths every day from heart disease, stroke and diabetes alone. These conditions are dizzyingly expensive. Cardiovascular disease costs $351 billion annually in health care spending and lost productivity, while diabetes costs $327 billion annually. The total economic cost of obesity is estimated at $1.72 trillion per year, or 9.3 percent of gross domestic product.
These human and economic costs are leading drivers of ever-rising health care spending, strangled government budgets, diminished competitiveness of American business and reduced military readiness.
Fortunately, advances in nutrition science and policy now provide a road map for addressing this national nutrition crisis. The “Food Is Medicine” solutions are win-win, promoting better well-being, lower health care costs, greater sustainability, reduced disparities among population groups, improved economic competitiveness and greater national security.
Some simple, measurable improvements can be made in several health and related areas. For example, Medicare, Medicaid, private insurers and hospitals should include nutrition in any electronic health record; update medical training, licensing and continuing education guidelines to put an emphasis on nutrition; offer patient prescription programs for healthy produce; and, for the sickest patients, cover home-delivered, medically tailored meals. Just the last action, for example, can save a net $9,000 in health care costs per patient per year.
Nutrition standards in schools, which have improved the quality of school meals by 41 percent, should be strengthened; the national Fresh Fruit and Vegetable Program should be extended beyond elementary schools to middle and high schools; and school garden programs should be expanded. And the Supplemental Nutrition Assistance Program, which supports grocery purchases for nearly one in eight Americans, should be leveraged to help improve diet quality and health.
Coordinated federal leadership and funding for research is also essential. This could include, for example, a new National Institute of Nutrition at the National Institutes of Health. Without such an effort, it could take many decades to understand and utilize exciting new areas, including related to food processing, the gut microbiome, allergies and autoimmune disorders, cancer, brain health, treatment of battlefield injuries and effects of nonnutritive sweeteners and personalized nutrition.
Finally, Government plays a crucial role. The significant impacts of the food system on well-being, health care spending, the economy and the environment — together with mounting public and industry awareness of these issues — have created an opportunity for government leaders to champion real solutions.
– by Dariush Mozaffarian, Dean, Tufts Friedman School of Nutrition Sciences and Policy
and Dan Glickman, Executive Director, Aspen Institute Congressional Program.
– This has been edited from an opinion piece that
originally appeared in the New York Times on Aug. 26, 2019
PEOPLE LIVING IN LOW INCOME COMMUNITIES have food access issues that can lead to a number of chronic diseases that are devastating. Fresh produce has been proven to produce better health outcomes for those who effectively increase their produce consumption. Instead of waiting until they require treatment, doctors can prescribe healthy food instead of medicine with the resources that result in affordable access to fresh food, and the knowledge to use it.
Here’s how it works: A patient is diagnosed as at-risk, and then qualifies for an intervention that includes the diagnosis from a prescriber, counseling from a nutritionist, basic nutrition and cooking education, and the financial incentive to purchase the produce. The “patient” participates in the programming, purchases and consumes more produce, then visits the clinic to check-in, adjust their healthy weight goals, and get a refill. — Michael Nischan, Founder of Wholesome Wave.
With the recent crisis in Flint, Michigan, it became clear that as a nation, we expect our cities to guarantee clean water to all people. When that doesn’t happen, we are rightfully indignant, yet it wasn’t always that way. It was only by the turn of the century, when the connection was made between cholera and clean water, that people started to view access to clean water as a public health issue.
We believe that we’re in that “cholera moment” now with food; the connections have been made between the “unclean” food that gets piped into communities of color, and the diet-related chronic illnesses that are plaguing these communities at astonishing rates.
Ward 8 has the highest rates of food-related chronic disease in the Washington, DC area, and only one grocery store for 85,000 people. In a community that battles alarming rates of violence, illiteracy, unemployment, and poverty, DC Greens, Giant Foods, AmeriHealth Caritas DC and DC Health have partnered to create the DC Produce Rx Program to positively impact the health outcomes of Ward 8 residents.
The program equips doctors with the tools to write prescriptions for fresh produce for low-income patients experiencing one of three chronic conditions—diabetes, prediabetes or hypertension—then combines food intervention with nutrition education to give ward residents confidence in making healthier food choices for themselves and their families.

This innovative initiative links food retailers, health care providers and Medicaid providers to create better access to fresh fruits and vegetables as well as nutrition and wellness opportunities for Medicaid patients experiencing or at risk for diet-related chronic diseases. While a number of other cities across the country are also administering similar programs, what makes DC’s program unique is their relationship to the largest Medicaid provider, AmeriHealth Caritas DC, and the access they’ve been granted to not only patient medical records but also claims data. This unprecedented access will provide the District with an opportunity to fully understand the ROI (e.g. ambulatory utilization, acute utilization, total cost of care) on a program such as this, with the goal being to show that it’s both good policy and good business to integrate Produce Rx Programs fully into healthcare systems. — Lauren Biel, Executive Director of DC Greens.
For food as medicine to become standard practice, a need exists for organizations willing to foster collaboration between partners that yearn to connect, yet lack the capacity to make it happen. Government agencies can certainly play a role, but on value of community-based organizations is their ability to incubate creative ideas that can eventually scale. In the early stages of any program, it’s necessary to be nimble, responsive and creative. Nonprofits are able to adjust faster, in order to perfect a program.
DC Greens, with financial support from DC Health and AmeriHealth Caritas, has put these principles into practice with the DC Produce Rx Program. DC Greens, in knowing that any meaningful systemic shift/solution requires weaving together previously unconnected players, focuses their work on the spaces between different sectors. In this case, they’ve brought together DC government, Medicaid payers, clinical partners, grocers, evaluators, and patients to create a system that can be sustainable for the long-run.
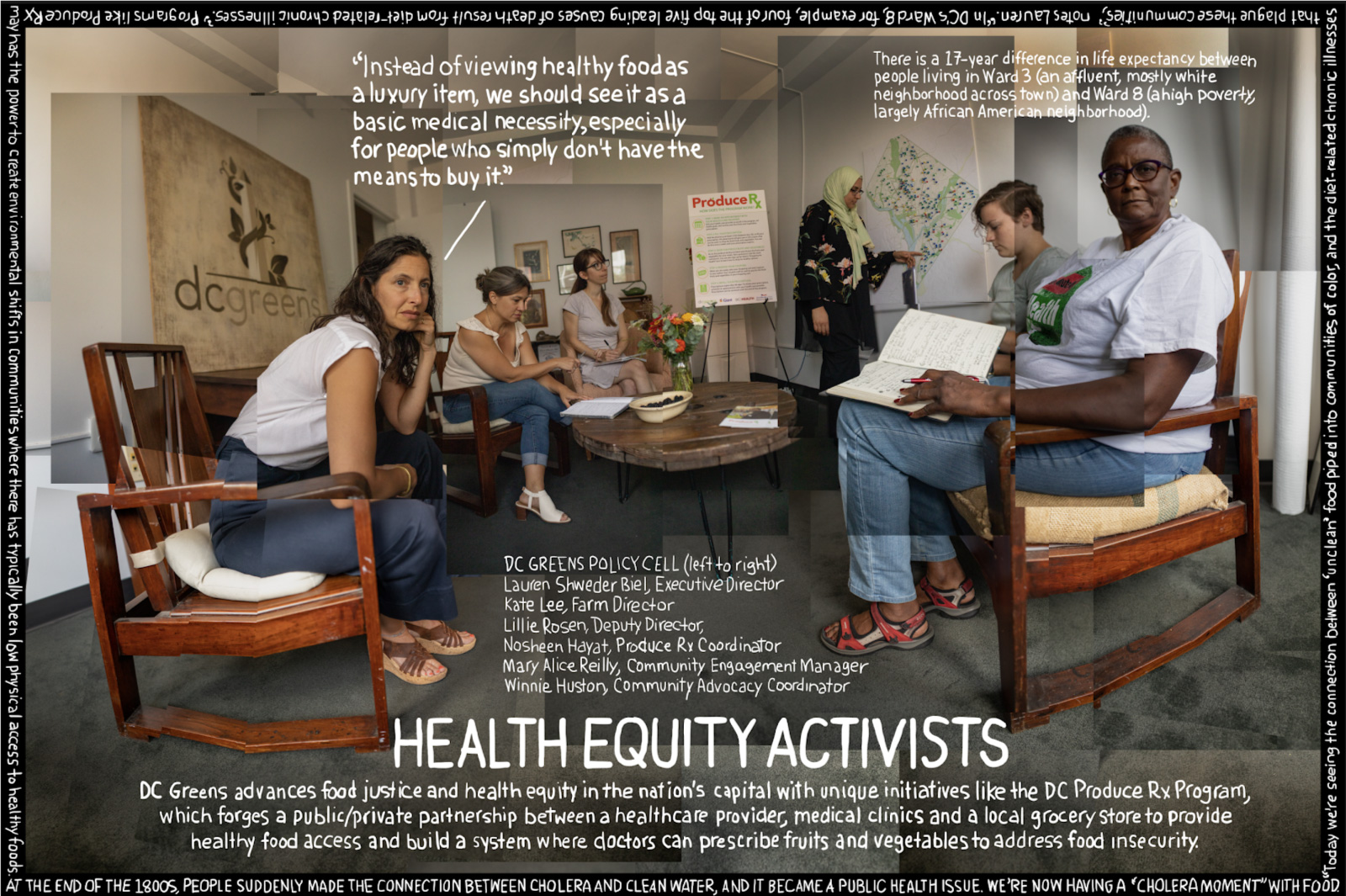
People often ask what our exact role is in the program, and the answer is: making it happen. We are living and working in a city where there is a 17-year life expectancy difference between one area of the city (Ward 8, a high poverty, largely African American neighborhood) and Ward 3 (affluent, mostly white neighborhood across town). Four of the top five leading causes of death in Ward 8 diet-related chronic illnesses. The diabetes rates in Ward 8 are 5 times higher than in Ward 3. We know that people in both communities want healthy food, but in Ward 8 they simply don’t have the means to buy it.
Building the pipe structure that connects clinical care with healthy food access requires DC Greens to juggle a variety of roles, from approaching partners and raising funds, to figuring out workflows and a proving return on investment, all to prove out a model that show where doctors prescribe fruits and vegetables to food insecure patients as a matter of course.
DC Greens also believes that a program like Produce Rx can help healthcare providers support local economies, with the added benefit of building new markets that can remove the risk for grocers with thin profit margins, and encourage them to carry more fruit and vegetables.
AmeriHealth Caritas DC is the managed care organization (MCO) for patients enrolled in the DC Produce Rx Program. Their interest is to see increased visits to a patient’s primary care practitioner (PCP), improved health biomarkers, and a reduction in ER admissions.

Given the increased relevance of social determinants, it’s become fashionable to say that your zip code says more about your health outcome than a genetic test, which may explain the pivotal role that a DC-based data-analytics firm plays in the DC Produce Rx program.
Socially Determined takes that analogy a step further by using highly refined tools that can look at social determinants of health not on a community level or even by zip code, but literally block by block, house by house, to help healthcare providers assess risk. They combine community-level contextual data from their national repository of social determinants of health (SDOH) data with risk scores captured from individual-level clinical, claims, screening, and programmatic data. This allows them to help clients like Amerihealth Caritas identify SDOH risks at the domain-level (e.g., food insecurity, crime, and housing instability) for the communities and populations the healthcare provider serves.
Harnessing the power of their tools will provide a groundbreaking new approach for evaluating the impact of the Produce Rx intervention on claims level outcomes. Measuring the specific quality and financial ROI implications of the program, and performing a comparative ROI analysis of various integration models of Produce Rx, will hopefully be key drivers to convince other health insurance companies of the viability of this initiative.
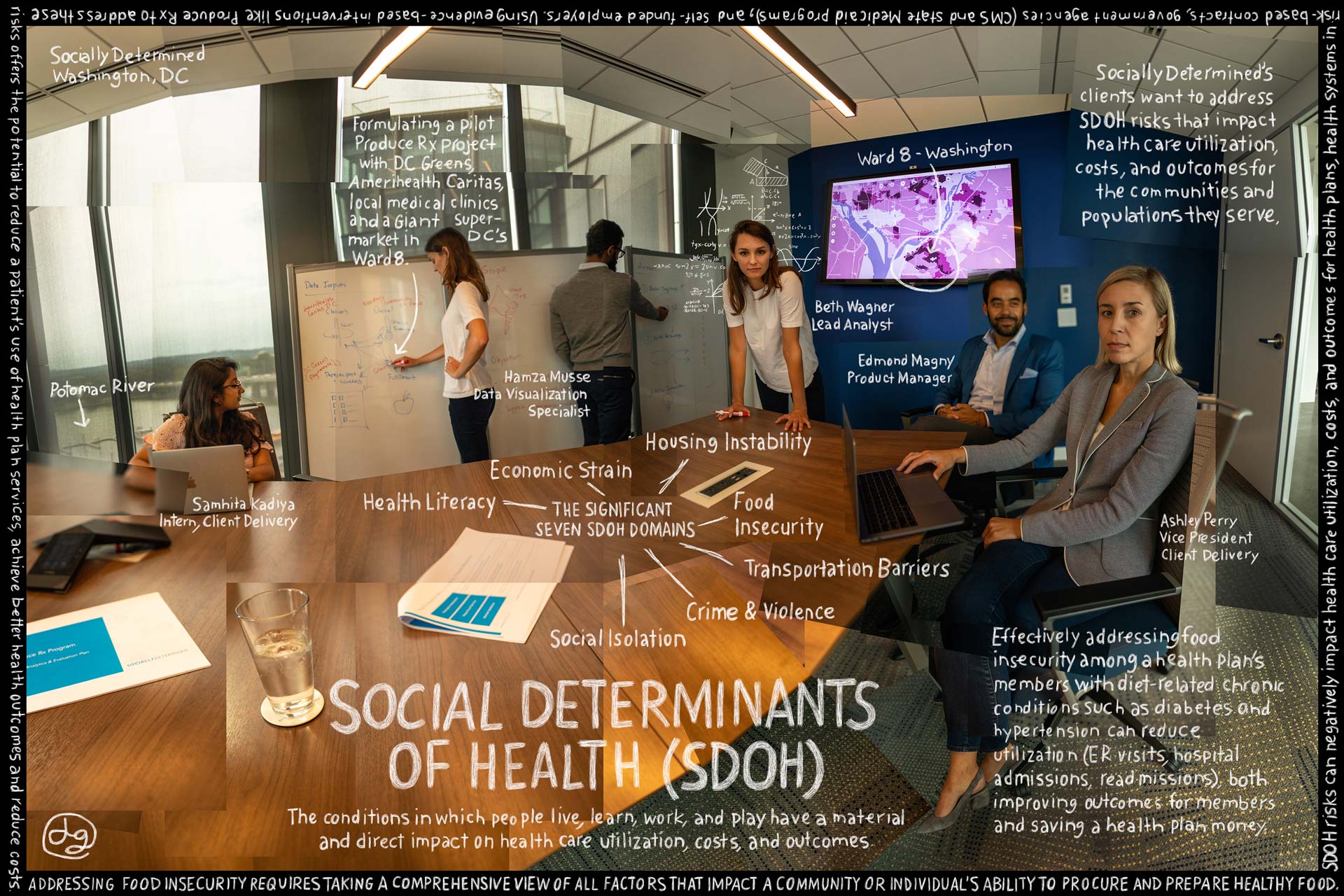
Socially Determined began their work on the program by integrating three years of encounter-based EMR data into their analytic platform. This enabled them to analyze utilization patterns, chronic disease burdens, and other relevant clinical factors in their analysis. For their Produce Rx evaluation, they are focused on a more limited set of biometric data, which includes height, weight, BMI, A1c, and blood pressure for program participants for each clinical encounter during the intervention.
In every community and population Socially Determined has analyzed to date, food insecurity remains one of the most consistently impactful domains in terms of its correlation to elevated social risk, increased utilization and cost.
At the close of this pilot program, Socially Determined will deliver a full evaluation report to the program partners that quantifies the impact of the intervention clinically, financially, and experientially. Their analysis of the claims data during this program may also provide key findings that help explain the role a Produce Prescription model can play as an evidence-based intervention that addresses food access and affordability, both of which are key drivers of food insecurity risk. Their strategic recommendations may also suggest additional communities or populations that could benefit from the program and/or potential refinements to the program design that would maximize impact and ROI.
Community of Hope is one of three Federally Qualified Health Centers offering Produce Rx to AmeriHealth Patients in Ward 8. Their care coordinators enroll patients in the program and call prescriptions into the Giant pharmacy.
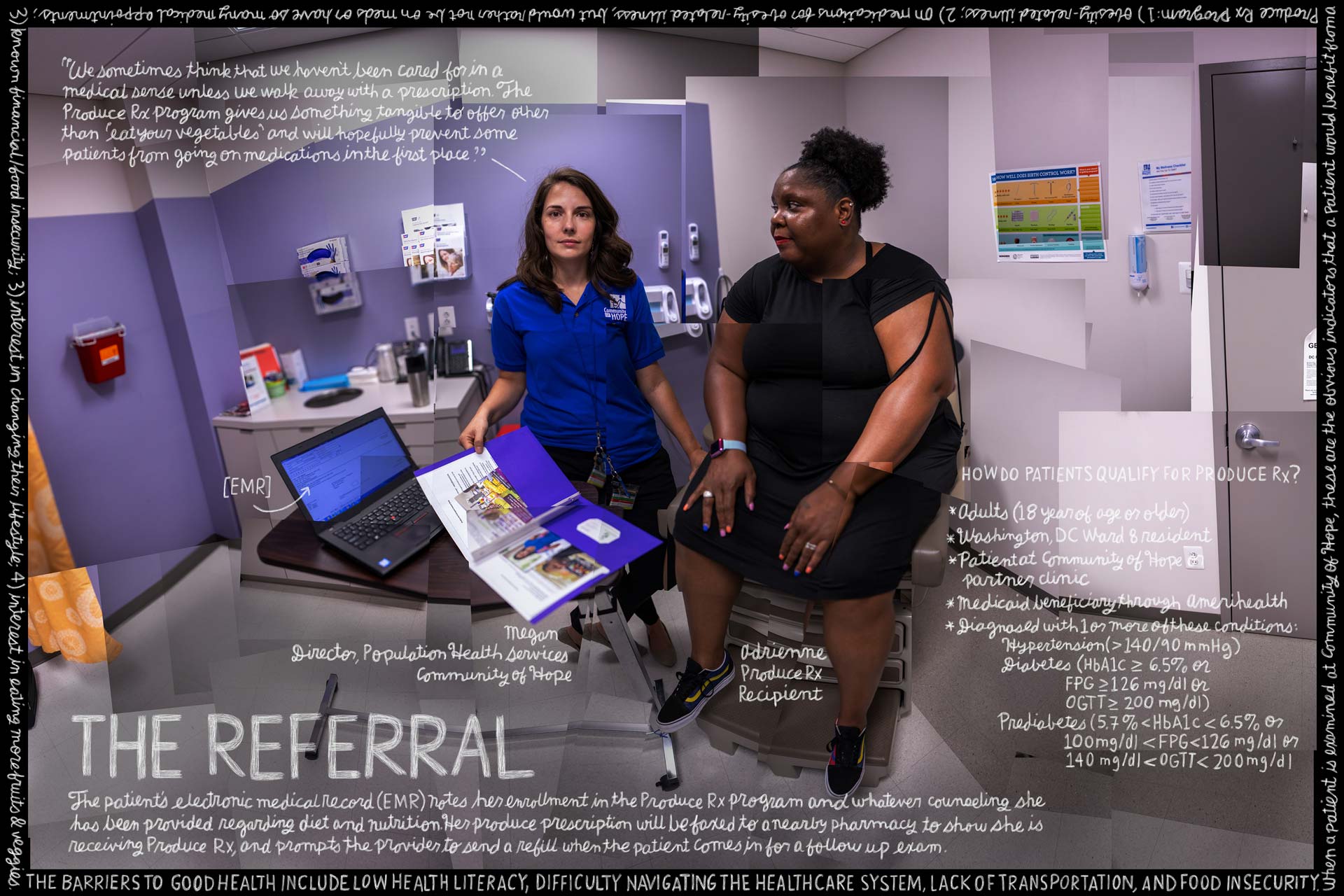
Community of Hope believes that the best way to improve health outcomes is to meet people where they are, listen to what’s getting in the way of their health (taking care of everyone else, distrust of healthcare system, trauma, lack of resources, etc.), and build trust by meeting those needs with compassion and high quality services and referrals.
Produce Rx is an important new tool for addressing the barriers to good health, which include low health literacy, difficulty navigating the healthcare system, lack of transportation, and food insecurity.
After an Ameri-Health Caritas member is prescreened by a medical clinic worker for type 2 diabetes, pre-diabetes, or hypertension, and is also found to be food insecure, they become eligible to participate in the Produce Rx program. They are referred to the Giant pharmacy in DC’s Ward 8, where they consult with a pharmacist, obtain medications prescribed by their physician and receive a 20 dollar weekly voucher for free produce. Anchoring the Produce Rx program in the supermarket’s pharmacy helps participants shift how they see the role food plays in their personal health by showing them that “food” is a medicine, just like any other pill.
In areas with patients on fixed incomes, the Produce Rx program allows patients to better allocate their resources, and make smarter food choices, which even means experimenting with produce, which has a decreased shelf-life when compared to non-perishables. “We’ve positioned ourselves as a healthcare destination within the store for all our customers,” says Giant Pharmacist Samir Balile.
“Pharmacy is a changing field,” Samir explains. “First, pharmacists are the most accessible healthcare provider. There’s no copay, short wait times, free professional advice, and we’re open 7 days a week! Second, we turn patient contacts into opportunities to make important clinical interventions. Pharmacist can identify gaps in patient care, provide immunizations, educate patients and emphasize the importance of medication adherence, as well as other potential adherence deterrents patients may be experiencing with their medications regimens. These are tasks that pharmacist complete daily that minimize healthcare costs such as hospitalizations, acute illness and more medications to mitigate undesired side-effects.
Can he explain how medication compliance works, and why Produce Rx is a valuable tool to support this?
“Pharmacies are now assessed by PDC (proportion of days covered),” Samir continues. “It’s a metric developed by insurance companies that dictates reimbursements based on patients’ adherence to their medication regimen (blood pressure, diabetes medications, cholesterol meds). From a pharmacy perspective, programs that incentivize individuals with free produce, both increase adherence and allow pharmacists to address any medication-related issues patients may be experiencing. From a retailer perspective, this program also increases foot traffic into the store and can drive further produce sales. It’s a win-win.”
The pharmacist then provides a warm hand-off to Giant’s in-store nutritionist, Jillian, who offers store-tours and free one-on-one counseling. Everything Jillian teaches helps to increase food literacy, from what to look for on a product label to manage weight, cholesterol, blood pressure, diabetes or overall wellness, to understanding the different roles of macro and micro nutrients. When people become confident in their daily decisions about food, they see changes in their health outcomes.
Giant’s nutritionists can be found in stores across Maryland, DC, and Virginia. While Jillian will meet any customer who makes an appointment, she often receives referrals from Giant pharmacists, local clinicians, and other community members. What questions is she asked most? How to read a product’s nutrition facts and how to determine the correct portion sizes, saturated fat, sugar or calories in the foods they should be eating.
Produce Rx is currently available at three health care centers across DC. While it’s too early in the program to see changes in health outcomes, data on program usage is available. 72% of participants are actively using the program, meaning that they have visited the pharmacy to fill their prescription at least once since enrollment. On average, 86% of vouchers that are distributed to participants on a monthly basis are used by participants to purchase fruits and vegetables.
In the long term, Produce Rx is expected to improve health-related outcomes relating to body-mass index, blood pressure, and blood glucose levels among individuals with pre-diabetes or diabetes. As patients visit their primary care physician more often to pick up their produce prescriptions, they have more frequent health check-ins and develop better relationships with their providers. As a result, Produce Rx is expected to decrease total health care expenditures and emergency care utilization costs among participating Medicaid patients. These cross-cutting findings have the potential to embed a ‘food as medicine’ approach across the local healthcare system by illustrating the role of food in shaping the social determinants of health. Produce Rx redefines fresh, healthy food as a critical component of clinical care, and offers a promising solution for sustainably improving patient health at a time when Medicaid providers, clinics, and hospital systems are searching for ways to lower rates of chronic disease and manage their costs
There are many ways to assess whether a program “works.” As pre-diabetic and diabetic patients change their relationship with food and get access to healthier diets, they will stabilize their conditions and engage more fully with their healthcare system.
With the DC Produce Rx Program, doctors have noted that they “finally have a way to help patients follow their medical advice.” Patients say that their diets have changed, and that they are modeling new behaviors for their children. At Giant, pharmacists say that are seeing patients more frequently, and their team is able to follow up with patients on their overall medication compliance. And with the unprecedented access to claims data gathered through the partnership between AmeriHealth Caritas and Socially Determined, cost savings on ER diversion, medication compliance, prevention of disease progression and much more can now being analyzed. Hopefully, capturing data from food is medicine initiatives like the DC Produce Rx program will lead to increased investment from the healthcare system in providing access to healthy food as a key component of prevention.
Allison Hess
Vice President, Health Innovation
GEISINGER
EATING THE RIGHT FOOD PLAYS AN IMPORTANT ROLE in overall health and the treatment of diet responsive conditions. By pairing fresh and nutritious food along with education and clinical services as part of a prescription-based program to their most at-risk patients with diabetes, Geisinger has improved patient outcomes while lowering per-patient costs.
Its Fresh Food Farmacy program provides qualifying patients with access to fresh, healthy, nutritious food, paired with education and clinical services, and more importantly empowers participants in the program to manage their medical conditions through food-related behavior and lifestyle changes.
To date, the program has shown that participating patients have 75% less hospital admissions, 30% less Emergency Room visits, and are more likely to close their preventive care gaps by having more regular visits with their primary care physician, when compared to a cohort population of those who participate but not enroll in the program. In addition, their participating patients with Type II Diabetes average a 2 point reduction in HbA1c, which when compared to already published literature could lead to a potential cost savings of $16,000-$24,000 per patient.
Geisinger Health Plan recently chose Scranton, PA as its third “Fresh Food Farmacy” location. A Community Needs assessment of the area identified alarming rates of diabetes coupled with increasing food insecurity statistics, with hunger, job security, transportation, and stable housing among the biggest social determinant issues that impact health outcomes for Scranton residents.
Without job security, individuals struggle to afford the food they need. Without reliable transportation and confronted by numerous food deserts, many patients rely on food service locations based on access that may not always offer the most nutritious food for themselves or their families. In cases where people are without stable housing, it becomes a challenge to store the food they can obtain from local food pantries.
Using food-as-medicine not only addresses food insecurity in these communities by providing patients and their families with a significant quantity of healthy, reliable food; it can also demonstrate how positive clinical impacts may help patients live healthier lives.
Providing increased awareness without judgement for these patients helps to strengthen a collaborative, community approach and serves as a catalyst to help patients better recognize the correlation between diet and health. This extensive education also includes grocery store tours, cooking demonstrations and group-based peer learning to help patients learn more about the impact of food on their diet responsive conditions.
There is a direct correlation between food security, literacy, and access and health outcomes. In particular, there is a bidirectional relationship between food insecurity and Type II Diabetes. Processed foods are big contributors to rising rates of diabetes and aggravate other chronic conditions. Maintaining a healthy weight and learning to better control autoimmune disorders are all interconnected in the battle against diabetes.
According to the Centers for Disease Control, by 2050, nearly 1 in 3 people in America will have type 2 diabetes. As a healthcare organization, Geisinger has invested heavily in the treatment of diabetes, yet despite the resources made available to their patients, they still saw an increase in the prevalence of uncontrolled diabetes. Lacking access to nutritious food as well as the awareness of how food impacts their chronic conditions often resulted in negative clinical results.
As Geisinger started to consider a fundamentally different approach to how they treated Type II diabetes, they recognized that without the proper food available for this diet responsive condition, patients would likely remain unmanaged and have further health complications.
Geisinger’s Fresh Food Farmacy program, while recognizing that a patient’s situation may change at any point during their journey, began annual screenings of EHRs (electronic health records) to identify patients who were both food insecure and suffered from uncontrolled Type 2 Diabetes (HBA1C levels greater than 8). Qualifying patients are referred for proactive reach out, can request to join, or are referred by their physician or other health care provider.
Each week, patients receive enough food to prepare healthy and nutritious meals for their whole family, twice a day for five days, utilizing recipes provided by Geisinger registered dieticians to encourage them to explore and prepare new healthy options on their own. Staples include fresh fruits; whole grains; lean proteins such as chicken, fish, turkey, pork, and vegetarian friendly entrees; and additional staple items within guides for diets with limited sodium, saturated fats, and carbohydrates.
By identifying the connection between food insecurity and adverse health outcomes, Geisinger developed a team-based approach to improving their patients’ health.
Patients often “give up” on trying to manage their diabetes, becoming complacent with poor health and frequent visits to the hospital become part of their routine. Breaking that cycle by providing a program where they can see the direct impact on their clinical outcomes, empowers patients in Geisinger’s program and not just benefits them physically and clinically, but also emotionally. They see the true benefits derived by developing a healthier diet.
When a participant first enrolls, baseline labs and biometric data are collected. Throughout the participant’s involvement in the program, markers are pulled to assess program effectiveness as well as identify any continued barriers or concerns, with the findings reviewed by the entire care team during Medical Home Meetings attended by the health coach, health manager, registered dietician, pharmacist, CHA, and other members of Geisinger’s leadership team.
Trends are continually assessed and solutions developed to target specific needs as well as tailor plans to ensure the patient has the proper tools to adequately self manage their condition.
To date, the program has shown that individuals who utilize the FFF have had 75% less admissions and 30% less ED rates than those of a similar cohort. They are also more likely to get preventive care gaps closed and have more regular visits with their primary care physician.
The program has also decreased A1C by 1-2 points, depending on the risk stratification of participants as well as their level of commitment to the program. The program has also captured an overall improvement in other health outcomes, including BMI, BP, LDL, and has assisted with care gap closure. Finally, Geisinger has also seen a transformation among patients who are now in control of their disease management (DM) rather than allowing DM to define them. Based on self-reported data, patients have also reported an increase in fruit and vegetable consumption, physical activity and improved overall health.
While each of their members has unique needs, Geisinger hopes that the ROI and patient outcome data they’re gathering with their multifaceted fresh food farmacy program will make it more likely for insurers to cover not only food as a benefit, but to provide clinical oversight utilizing coordinated clinical resources and the community-based organizations needed to help their members be successful long term.
Cathryn Couch
CEO
CERES COMMUNITY PROJECT
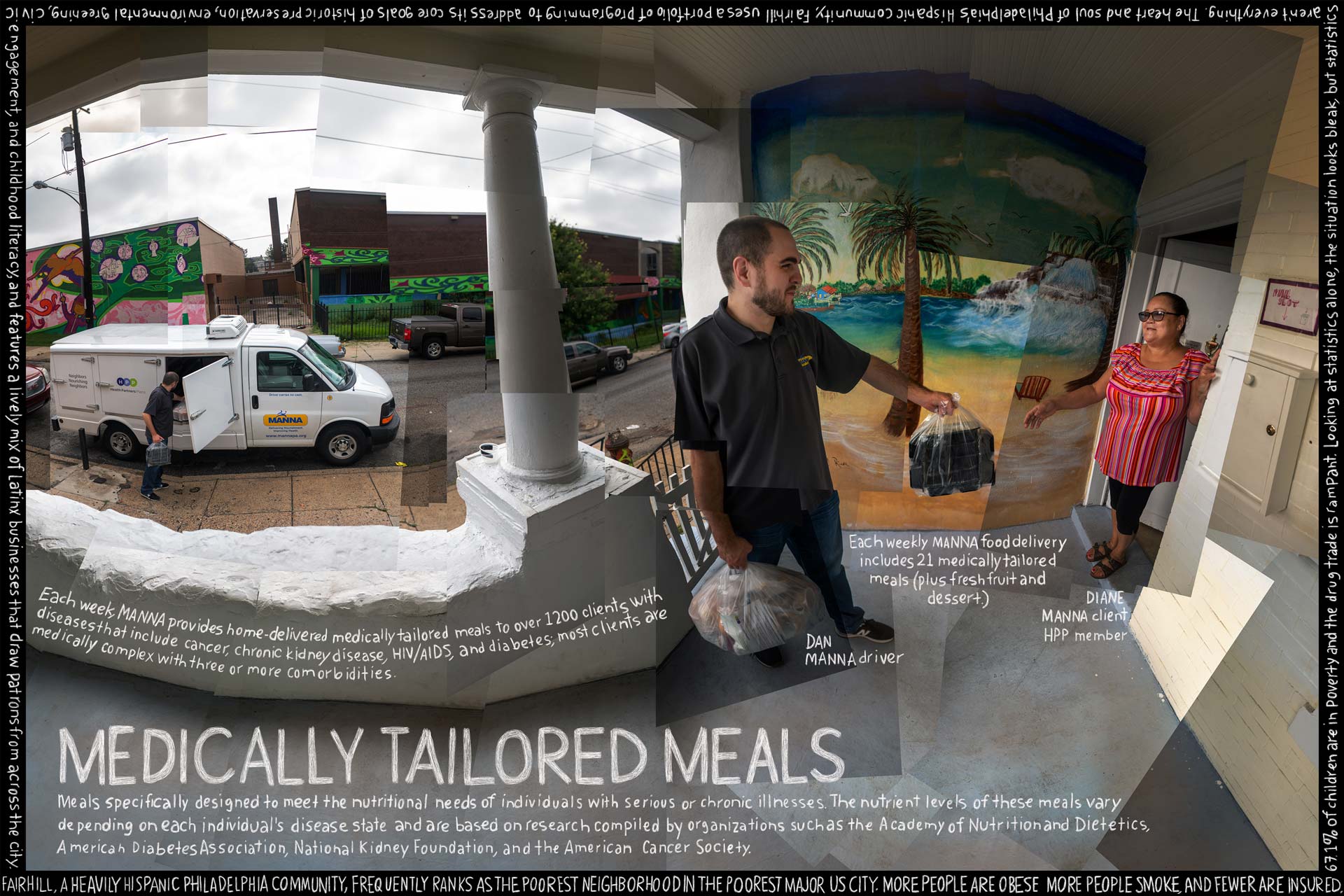
MEDICALLY TAILORED MEALS ARE ONE EXAMPLE of a food is medicine intervention. These are meals that are tailored to meet the unique nutritional needs of an individual based on their diagnos(e)s, as well as the additional complications that might come with that illness (i.e. treatment side effects, coexisting conditions , etc.). Research consistently shows that medically tailored meals improve health outcomes, lower the cost of care, and increase patient satisfaction.
Most often, medically tailored meals are provided through a referral from a medical professional or healthcare plan. A medically tailored meal intervention includes three elements: a medical referral, a nutritional assessment by a registered dietitian nutritionist (RDN) who also oversees the meal plan design, and the preparation and home-delivery of these meals. Patients also benefit from the human connection provided by the home delivery of these meals, with research indicating that medically tailored meals reduce isolation and loneliness, which can negatively impact health outcomes.
Most providers of medically tailored meals are community based organizations who are members of the Food is Medicine Coalition (FIMC). This group’s Clinical Committee has issued a sophisticated set of Medically Tailored Meal Nutrition Standards, based on research and more than 30 years of experience developing the science of medically tailoring meals. The Clinical Committee is made up of Registered Dietitian Nutritionists, who are experts in treating serious illness with nutrition.
A medically tailored meal intervention, as defined by the Food is Medicine Coalition , does not simply mean putting someone on a diet. FIMC clients’ medical lives are often complex – many are living with more than four serious illnesses at once – and they require an equally complex nutrition intervention. Medically tailored meals help the “sickest of the sick” in communities, often the 5% of patients that cost 50% of healthcare costs.
As well as having to manage a complex medical diet, many of the patients FIMC serves are too sick to shop or cook, and the majority are living at or below the federal poverty guideline meaning that their access to healthy food is severely limited.
Catherine McCarron
VP, Clinical Programs, Medicaid
HEALTH PARTNERS PLANS
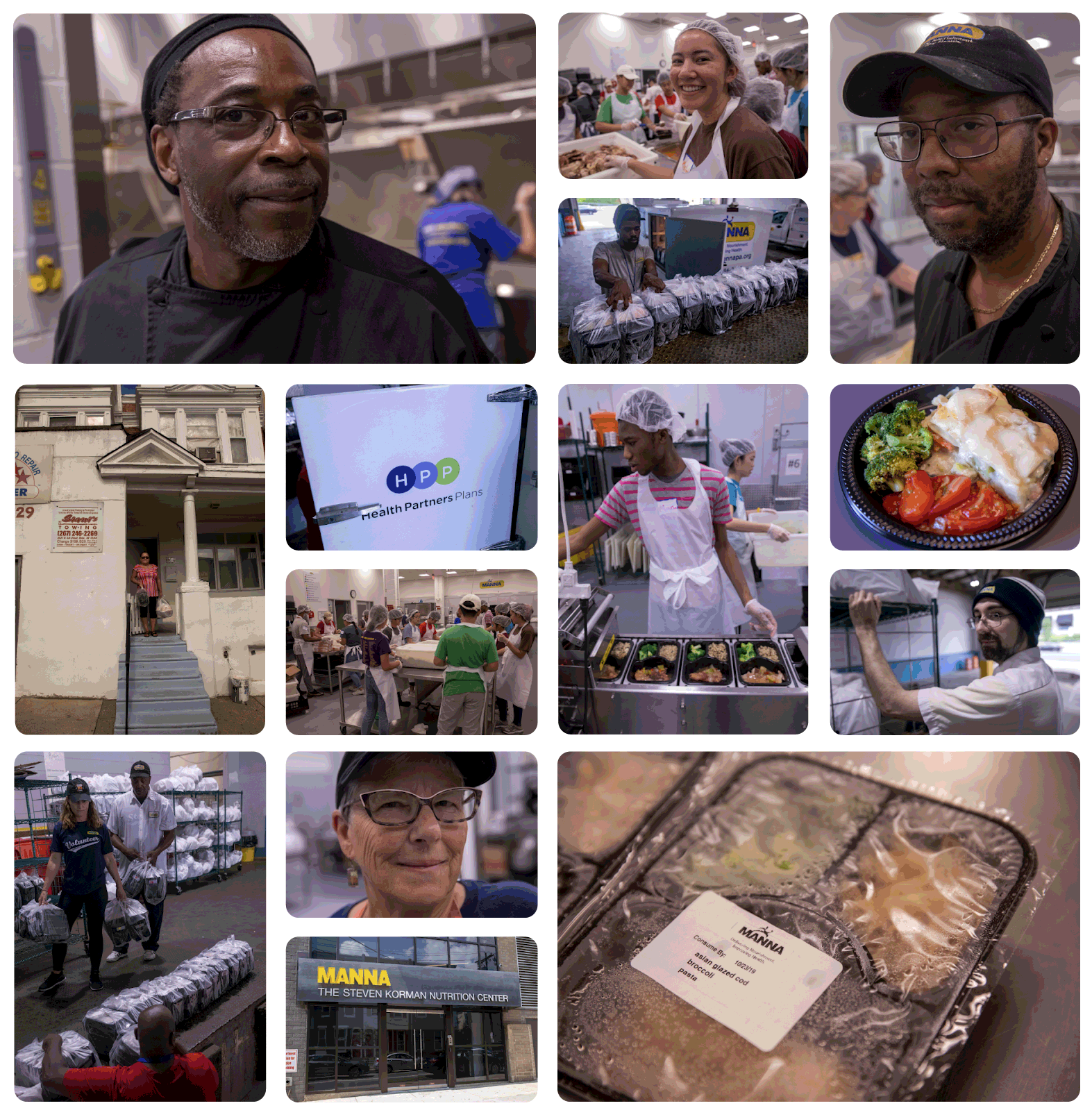
Founded more than 32 years ago, Health Partners Plans is a non-profit managed care organization in Greater Southeastern Pennsylvania that serves more than 250,000 members through its Medicaid, Medicare and Children’s Health Insurance Program (CHIP) plans. It is also one of the few MCOs in the nation that is hospital-owned.
In 2015, HPP and MANNA, a local community based organization, decided to explore a simple question: could they measure the positive health outcomes of members given therapeutic food as medicine to treat chronic health diseases? To find the answer, the HPP-MANNA Food is Medicine program began offering medically tailored meals and nutrition counseling to a small group of diabetic members.
After the program improved health outcomes and lowered costs per member per month, HPP expanded the program. As of October 2019, more than 730,600 meals have been delivered to more than 3,000 HPP members suffering from various illnesses, including diabetes, heart disease, malnutrition and kidney failure.
Findings for the population that ended services by January 1, 2019 show:
After the program improved health outcomes and lowered costs per member per month, HPP expanded the program. As of October 2019, more than 730,600 meals have been delivered to more than 3,000 HPP members suffering from various illnesses, including diabetes, heart disease, malnutrition and kidney failure.
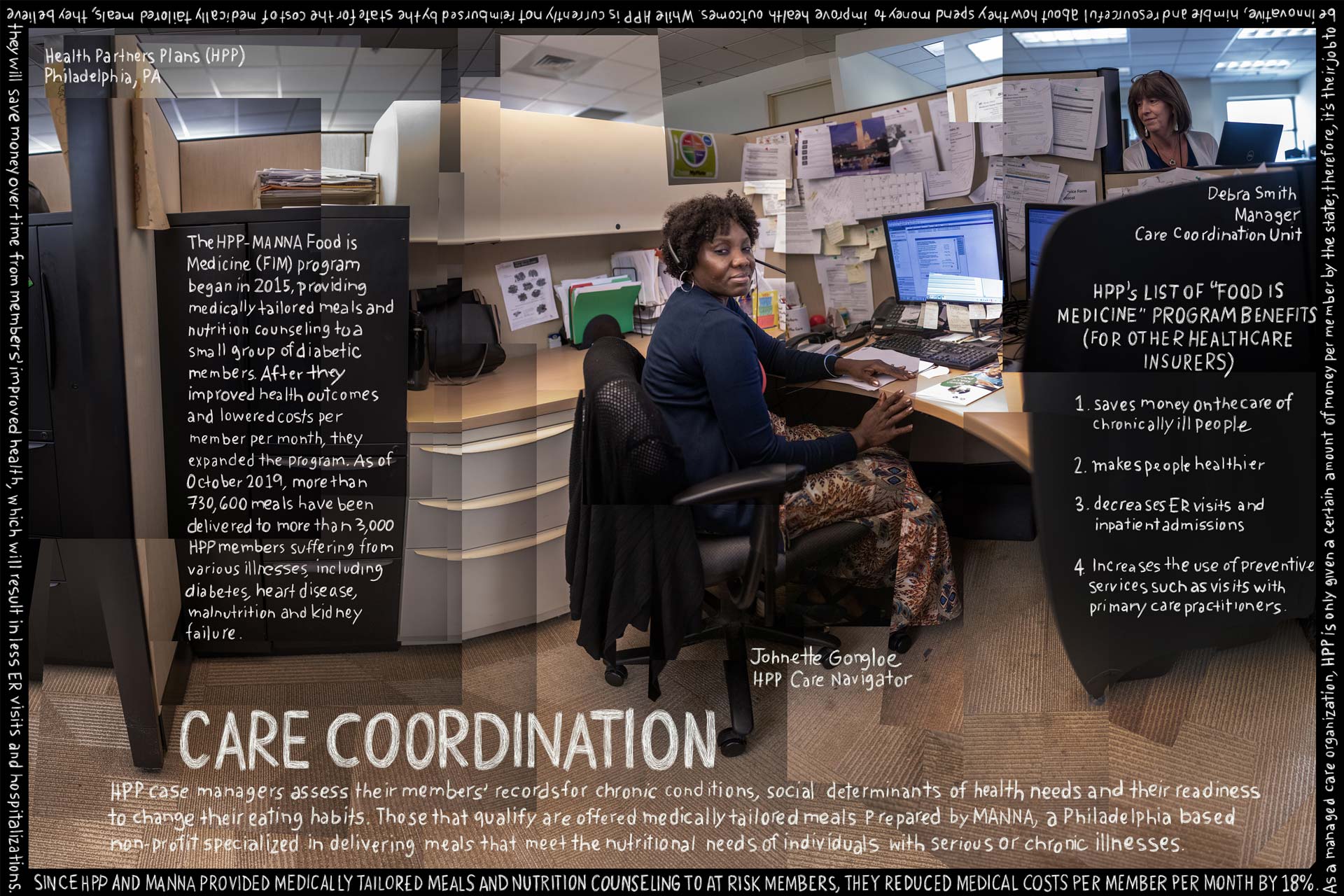
Today, the HPP-MANNA Food Is Medicine program has expanded to include members with other chronic illnesses, such as heart disease, malnutrition and kidney failure. Health Partners Plans views the Food Is Medicine (FIM) program as another tool to assist members with certain chronic conditions to self-manage their conditions. The FIM program also educates the member about how diet affects condition – something that is tangible instead of just words on paper or verbal communication from the healthcare providers.
By partnering with HPP, MANNA aims to demonstrate the value of medically tailored meals by providing members with therapeutic nutrition services that improve health and quality of life. The success of the MANNA-HPP partnership can spark changes in the healthcare landscape that ensure access to medically tailored meals for every individual with a health condition.
Sue Daugherty
CEO
METROPOLITAN AREA NEIGHBORHOOD NUTRITION ALLIANCE (MANNA)
MANNA was founded in 1990 by seven members of Philadelphia’s First Presbyterian Church in response to the HIV/AIDS epidemic. Initially, they provided care and comfort to those who were dying, but as HIV/AIDS treatments became available, they evolved to provide medically tailored meals for people with nutrition-impacted diseases and nutrition counseling to help people improve their health outcomes and quality of life.

Today, MANNA’s staff of licensed registered dietitians ensures that each medically tailored meal meets the unique and often complex nutritional needs of its clients. The nutrient levels of these meals vary depending on each individual’s disease state and are based on research compiled by organizations such as the Academy of Nutrition and Dietetics, American Diabetes Association, National Kidney Foundation, and the American Cancer Society.
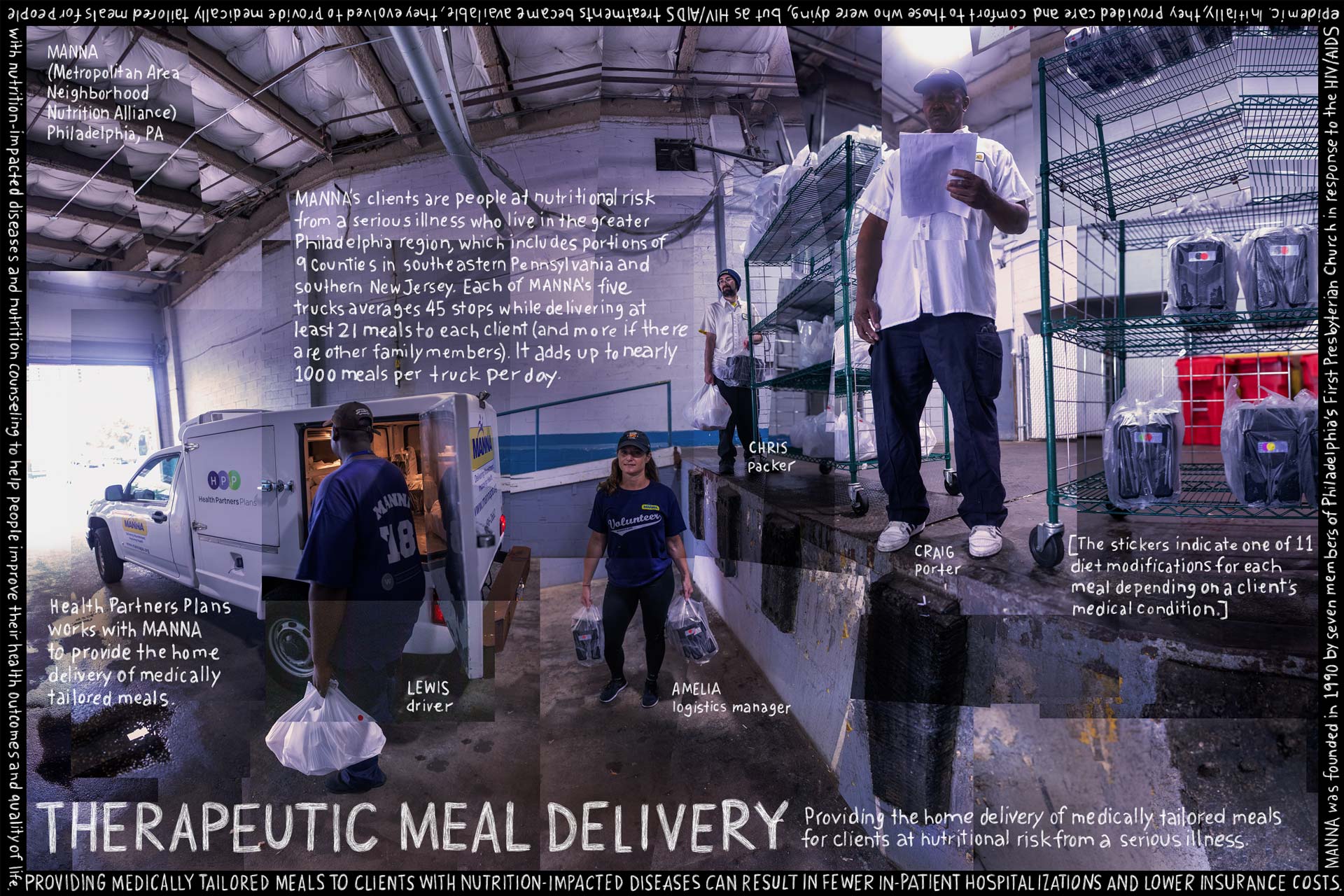

MANNA serves 1.3 million medically tailored meals each year in a delivery zone encompasses most of the nine (9) county Philadelphia and southern New Jersey region. While most clients reside in the metropolitan area, MANNA delivery drivers cover over 1,000 square miles in the surrounding region. For those residing outside the delivery zone, MANNA recently expanded a shipping program via an insurance partner that allows the organization to reach members residing across the state of Pennsylvania.
Sharing the successful outcomes of the HPP-MANNA Food Is Medicine partnership may convince healthcare insurers that investing in medically tailored meals for chronically ill people may save money in the long run, as people may become healthier, and their utilization of services (ER visits and inpatient admissions) decreases while their use of preventive services, such as PCP visits, continues.
David Eisenberg
Director
TEACHING KITCHEN COLLABORATIVE
THE TERM “TEACHING KITCHEN” elicits images of stainless steel kitchens used by students learning techniques to make food delicious. Within the context of Food Is Medicine, however, teaching kitchens are more than just a place used to teach culinary techniques. They are a “learning laboratory” aimed at changing lifestyle behaviors to ultimately improve one’s health (and thereby help decrease costs related to disease management as well as disease prevention and health maintenance).
Today’s teaching kitchens, which already exist in hospitals, medical schools, corporate worksites, colleges, K-12 schools, retirement facilities, YMCA’s and across the US VA system, typically include most or all of the following educational components:
Some teaching kitchens are “built-in”, whereas others are “pop-ups” or “mobile” and therefore less costly. Dozens currently exist and hundreds more are being planned across the US and globally. Importantly, all include more than just a “kitchen.”
The 30+ teaching kitchens associated with the Teaching Kitchen Collaborative are working to collectively develop best practices and to demonstrate, through research, that teaching kitchen curricula have the potential to predictably- and sustainably- change self-care behaviors, health outcomes, and, ultimately, the cost of health care, and quality of life, for patients, employees, students, families and society at large.
Olivia Weinstein
Culinary Nutrition Manager MS,RD,LDN
BOSTON MEDICAL CENTER
The Teaching Kitchen at Boston Medical Center (BMC) serves thousands of patients each year and hosts an average of 25 classes per month for patients with obesity, hypertension, cancer, chronic kidney disease, chronic pain, substance use disorder, disabilities, and more. The Teaching Kitchen also partners with department support groups to provide culinary and nutritional education for patients with type 2 diabetes, pregnant moms, and bariatric weight loss surgery preparation. Patients learn how to help treat and manage their conditions by first recognizing the importance of eating whole and healthy foods and second developing the necessary culinary skills to prepare their own nourishing meals utilizing food from the BMC food pantry.
A number of initiatives also provide culinary education for young people, including a summer camp with children from 10 different public schools in Boston, a class for families called “Family Fun with Food”, and a class for teenagers called “Teen Battle Chef”.
The teaching kitchen also offers team-building classes for various departments at BMC, culinary skills classes, and classes for healthcare professionals, including an “Eat to Treat” program for first year medical students at the Boston University School of Medicine.
Dietitians and physicians can also refer patients, as part of their treatment plans, to attend classes at the Teaching Kitchen. Research studies are currently underway with Boston Medical Center’s Endocrinology, Obstetrics and Gynecology departments, as well as investigating the overall efficacy of using teaching kitchens as an integrative intervention.
Follow our latest activities and learn more about how you can take part in your own community.
Our work depends on contributions by people like you. If you like what you see, you can support us here!
We’d love to hear from you! Contact us with general questions or media requests.
This website was built by The Lexicon™, a 501(c)(3) tax-exempt nonprofit organization headquartered in Petaluma, CA.
Check out our Privacy Policy, Cookie Policy, and Terms of Use.
© 2023 – The Lexicon™
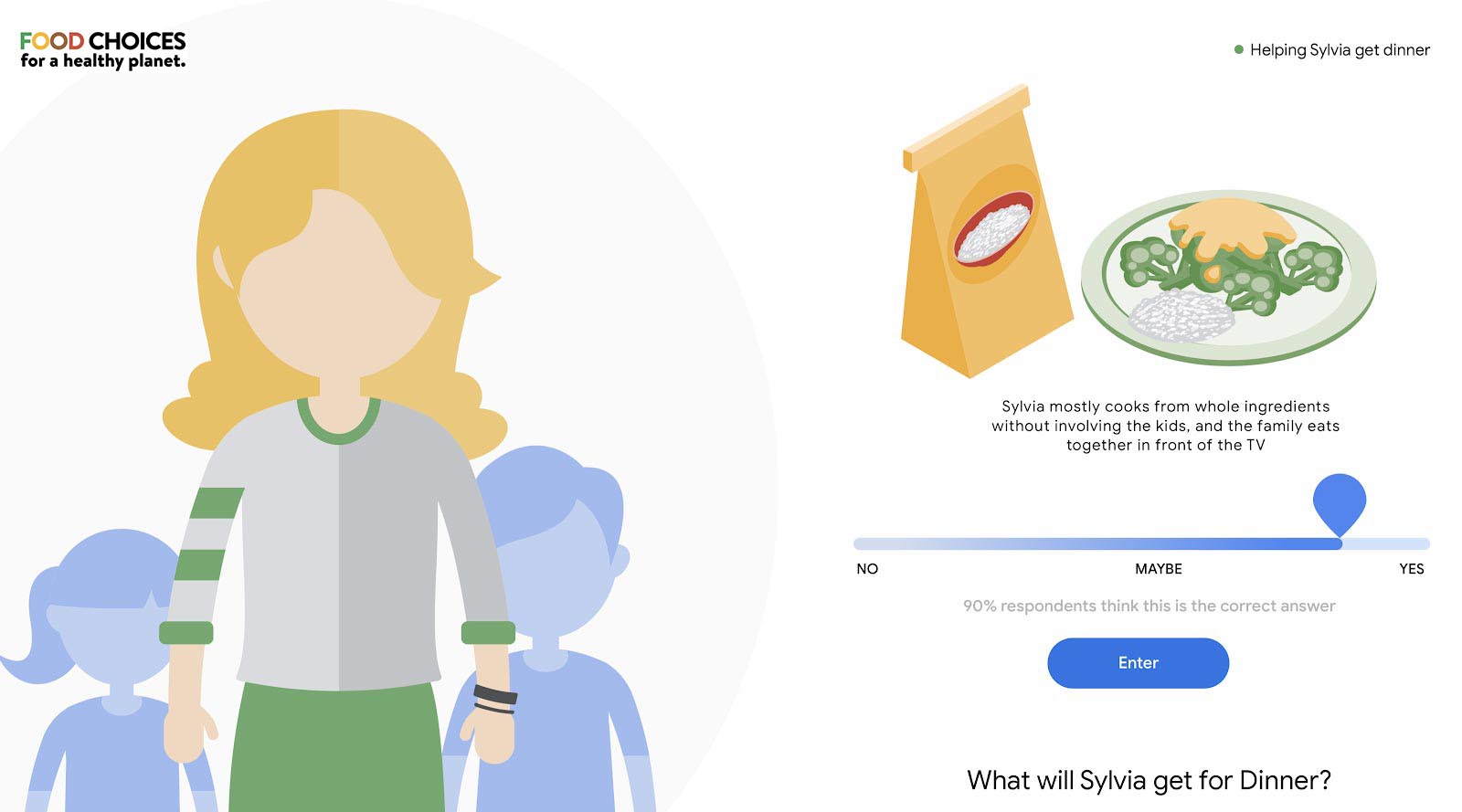
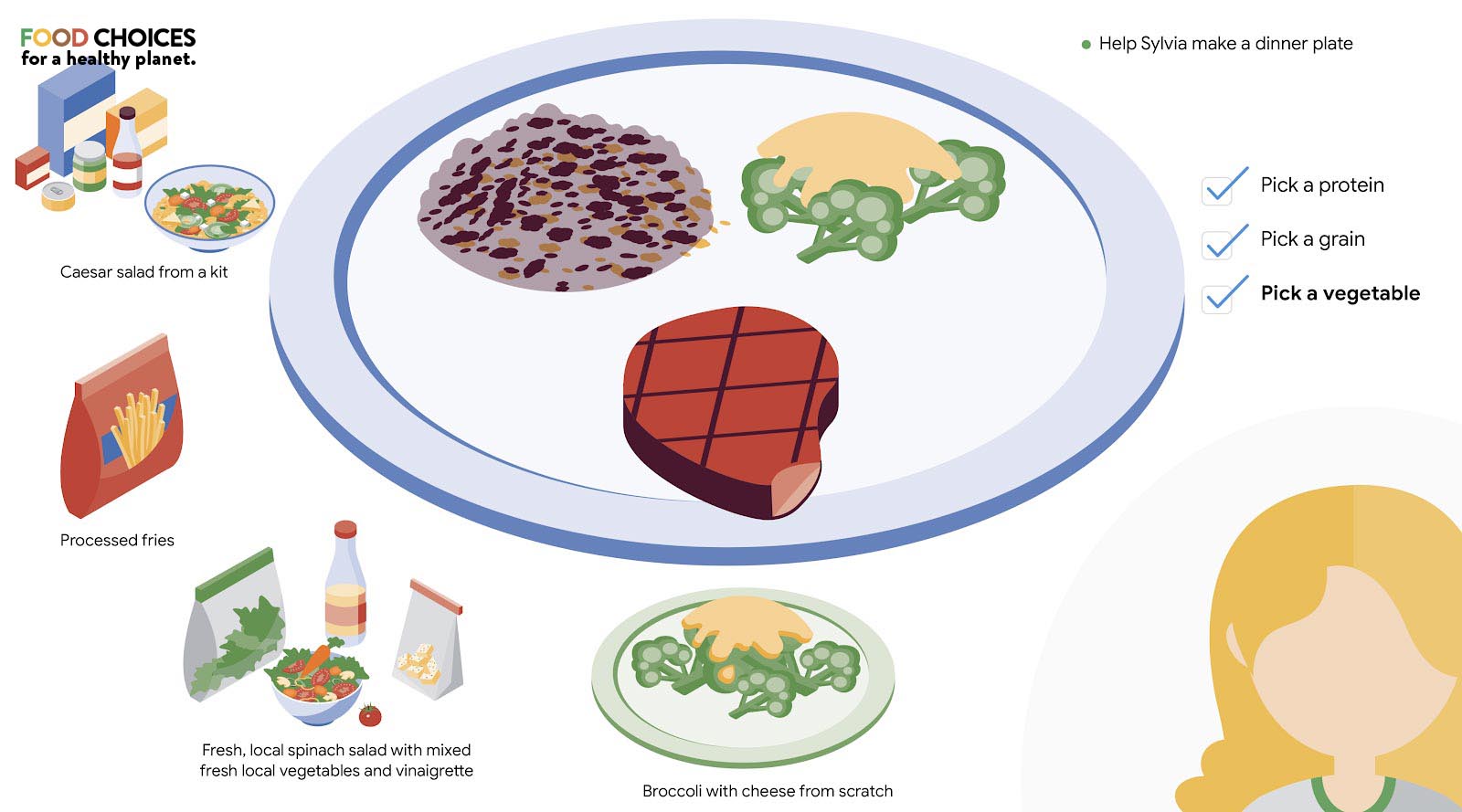
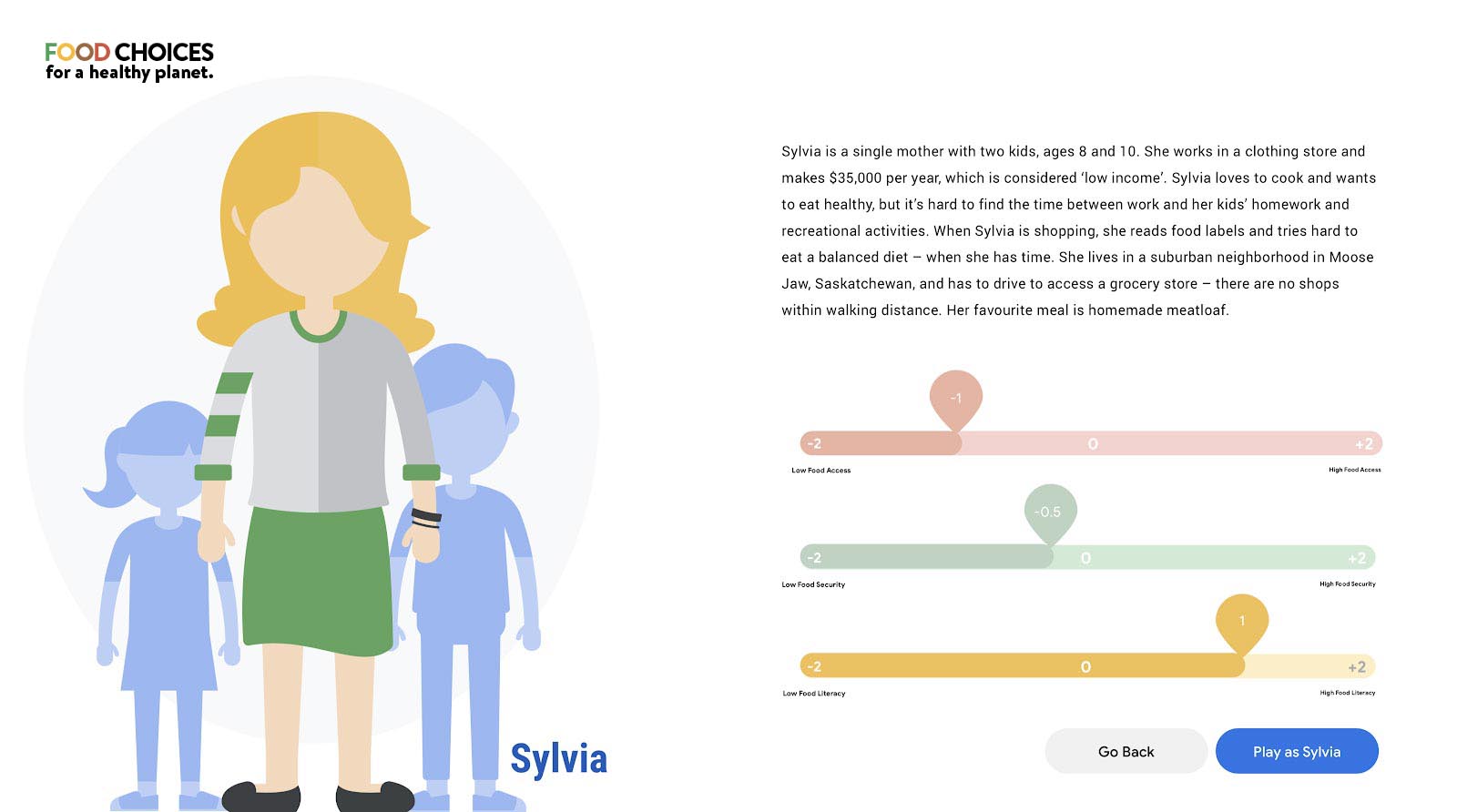
This game was designed to raise awareness about the impacts our food choices have on our own health, but also the environment, climate change and the cultures in which we live.
First, you can choose one of the four global regions and pick a character that you want to play.
Each region has distinct cultural, economic, historical, and agricultural capacities to feed itself, and each character faces different challenges, such as varied access to food, higher or lower family income, and food literacy.
As you take your character through their day, select the choices you think they might make given their situation.
At the end of the day you will get a report on the impact of your food choices on five areas: health, healthcare, climate, environment and culture. Take some time to read through them. Now go back and try again. Can you make improvements in all five areas? Did one area score higher, but another score lower?
FOOD CHOICES FOR A HEALTHY PLANET will help you better understand how all these regions and characters’ particularities can influence our food choices, and how our food choices can impact our personal health, national healthcare, environment, climate, and culture. Let’s Play!
The FOOD CHOICES FOR A HEALTHY PLANET game allows users to experience the dramatic connections between food and climate in a unique and engaging way. The venue and the game set-up provides attendees with a fun experience, with a potential to add a new layer of storytelling about this topic.
Starting the game: the pilot version of the game features four country/regions: Each reflects a different way people (and the national dietary guidelines) look at diets: Nordic Countries (sustainability), Brazil (local and whole foods instead of ultra-processed foods); Canada (plant-forward), and Indonesia (developing countries).
Personalizing the game: players begin by choosing a country and then a character who they help in making food choices over the course of one day. Later versions may allow for creating custom avatars.
Making tough food choices: This interactive game for all ages shows how the food choices we make impact our health and the environment, and even contribute to climate change.

What we eat matters: at the end of each game, players learn that every decision they make impacts not only their health, but a national healthcare system, the environment, climate and even culture.
We’d love to know more about you and why you think you will be a great fit for this position! Shoot us an email introducing you and we’ll get back to you as soon as possible!
Providing best water quality conditions to ensure optimal living condition for growth, breeding and other physiological needs
Water quality is sourced from natural seawater with dependency on the tidal system. Water is treated to adjust pH and alkalinity before stocking.
Producers that own and manages the farm operating under small-scale farming model with limited input, investment which leads to low to medium production yield
All 1,149 of our farmers in both regencies are smallholder farmers who operate with low stocking density, traditional ponds, and no use of any other intensification technology.
Safe working conditions — cleanliness, lighting, equipment, paid overtime, hazard safety, etc. — happen when businesses conduct workplace safety audits and invest in the wellbeing of their employees
Company ensure implementation of safe working conditions by applying representative of workers to health and safety and conduct regular health and safety training. The practices are proven by ASIC standards’ implementation
Implementation of farming operations, management and trading that impact positively to community wellbeing and sustainable better way of living
The company works with local stakeholders and local governments to create support for farmers and the farming community in increasing resilience. Our farming community is empowered by local stakeholders continuously to maintain a long generation of farmers.
Freezing seafood rapidly when it is at peak freshness to ensure a higher quality and longer lasting product
Our harvests are immediately frozen with ice flakes in layers in cool boxes. Boxes are equipped with paper records and coding for traceability. We ensure that our harvests are processed with the utmost care at <-18 degrees Celsius.
Sourcing plant based ingredients, like soy, from producers that do not destroy forests to increase their growing area and produce fish feed ingredients
With adjacent locations to mangroves and coastal areas, our farmers and company are committed to no deforestation at any scale. Mangrove rehabilitation and replantation are conducted every year in collaboration with local authorities. Our farms are not established in protected habitats and have not resulted from deforestation activity since the beginning of our establishment.
Implement only natural feeds grown in water for aquatic animal’s feed without use of commercial feed
Our black tiger shrimps are not fed using commercial feed. The system is zero input and depends fully on natural feed grown in the pond. Our farmers use organic fertilizer and probiotics to enhance the water quality.
Enhance biodiversity through integration of nature conservation and food production without negative impact to surrounding ecosysytem
As our practices are natural, organic, and zero input, farms coexist with surrounding biodiversity which increases the volume of polyculture and mangrove coverage area. Farmers’ groups, along with the company, conduct regular benthic assessments, river cleaning, and mangrove planting.
THE TERM “MOONSHOT” IS OFTEN USED TO DESCRIBE an initiative that goes beyond the confines of the present by transforming our greatest aspirations into reality, but the story of a moonshot isn’t that of a single rocket. In fact, the Apollo program that put Neil Armstrong on the moon was actually preceded by the Gemini program, which in a two-year span rapidly put ten rockets into space. This “accelerated” process — with a new mission nearly every 2-3 months — allowed NASA to rapidly iterate, validate their findings and learn from their mistakes. Telemetry. Propulsion. Re-entry. Each mission helped NASA build and test a new piece of the puzzle.
The program also had its fair share of creative challenges, especially at the outset, as the urgency of the task at hand required that the roadmap for getting to the moon be written in parallel with the rapid pace of Gemini missions. Through it all, the NASA teams never lost sight of their ultimate goal, and the teams finally aligned on their shared responsibilities. Within three years of Gemini’s conclusion, a man did walk on the moon.
FACT is a food systems solutions activator that assesses the current food landscape, engages with key influencers, identifies trends, surveys innovative work and creates greater visibility for ideas and practices with the potential to shift key food and agricultural paradigms.
Each activator focuses on a single moonshot; instead of producing white papers, policy briefs or peer-reviewed articles, these teams design and implement blueprints for action. At the end of each activator, their work is released to the public and open-sourced.
As with any rapid iteration process, many of our activators re-assess their initial plans and pivot to address new challenges along the way. Still, one thing has remained constant: their conviction that by working together and pooling their knowledge and resources, they can create a multiplier effect to more rapidly activate change.
Co-Founder
THE LEXICON
Vice President
Global Workplace Programs
GOOGLE
Who can enter and how selections are made.
A Greener Blue is a global call to action that is open to individuals and teams from all over the world. Below is a non-exhaustive list of subjects the initiative targets.
To apply, prospective participants will need to fill out the form on the website, by filling out each part of it. Applications left incomplete or containing information that is not complete enough will receive a low score and have less chance of being admitted to the storytelling lab.
Nonprofit organizations, communities of fishers and fish farmers and companies that are seeking a closer partnership or special support can also apply by contacting hello@thelexicon.org and interacting with the members of our team.
Special attention will be given to the section of the form regarding the stories that the applicants want to tell and the reasons for participating. All proposals for stories regarding small-scale or artisanal fishers or aquaculturists, communities of artisanal fishers or aquaculturists, and workers in different steps of the seafood value chain will be considered.
Stories should show the important role that these figures play in building a more sustainable seafood system. To help with this narrative, the initiative has identified 10 principles that define a more sustainable seafood system. These can be viewed on the initiative’s website and they state:
Seafood is sustainable when:
Proposed stories should show one or more of these principles in practice.
Applications are open from the 28th of June to the 15th of August 2022. There will be 50 selected applicants who will be granted access to The Lexicon’s Total Storytelling Lab. These 50 applicants will be asked to accept and sign a learning agreement and acceptance of participation document with which they agree to respect The Lexicon’s code of conduct.
The first part of the lab will take place online between August the 22nd and August the 26th and focus on training participants on the foundation of storytelling, supporting them to create a production plan, and aligning all of them around a shared vision.
Based on their motivation, quality of the story, geography, and participation in the online Lab, a selected group of participants will be gifted a GoPro camera offered to the program by GoPro For A Change. Participants who are selected to receive the GoPro camera will need to sign an acceptance and usage agreement.
The second part of the Storytelling Lab will consist of a production period in which each participant will be supported in the production of their own story. This period goes from August 26th to October 13th. Each participant will have the opportunity to access special mentorship from an international network of storytellers and seafood experts who will help them build their story. The Lexicon also provides editors, animators, and graphic designers to support participants with more technical skills.
The final deadline to submit the stories is the 14th of October. Participants will be able to both submit complete edited stories, or footage accompanied by a storyboard to be assembled by The Lexicon’s team.
All applicants who will exhibit conduct and behavior that is contrary to The Lexicon’s code of conduct will be automatically disqualified. This includes applicants proposing stories that openly discriminate against a social or ethnic group, advocate for a political group, incite violence against any group, or incite to commit crimes of any kind.
All submissions must be the entrant’s original work. Submissions must not infringe upon the trademark, copyright, moral rights, intellectual rights, or rights of privacy of any entity or person.
Participants will retain the copyrights to their work while also granting access to The Lexicon and the other partners of the initiative to share their contributions as part of A Greener Blue Global Storytelling Initiative.
If a potential selected applicant cannot be reached by the team of the Initiative within three (3) working days, using the contact information provided at the time of entry, or if the communication is returned as undeliverable, that potential participant shall forfeit.
Selected applicants will be granted access to an advanced Storytelling Lab taught and facilitated by Douglas Gayeton, award-winning storyteller and information architect, co-founder of The Lexicon. In this course, participants will learn new techniques that will improve their storytelling skills and be able to better communicate their work with a global audience. This skill includes (but is not limited to) how to build a production plan for a documentary, how to find and interact with subjects, and how to shoot a short documentary.
Twenty of the participants will receive a GoPro Hero 11 Digital Video and Audio Cameras by September 15, 2022. Additional participants may receive GoPro Digital Video and Audio Cameras to be announced at a later date. The recipients will be selected by advisors to the program and will be based on selection criteria (see below) on proposals by Storytelling Lab participants. The selections will keep in accordance with Lab criteria concerning geography, active participation in the Storytelling Lab and commitment to the creation of a story for the Initiative, a GoPro Camera to use to complete the storytelling lab and document their story. These recipients will be asked to sign an acceptance letter with terms of use and condition to receive the camera.
The Lexicon provides video editors, graphic designers, and animators to support the participants to complete their stories.
The submitted stories will be showcased during international and local events, starting from the closing event of the International Year of Fisheries and Aquaculture 2022 in Rome, in January 2023. The authors of the stories will be credited and may be invited to join.
Storytelling lab participation:
Applicants that will be granted access to the storytelling Lab will be evaluated based on the entries they provided in the online form, and in particular:
Applications will be evaluated by a team of 4 judges from The Lexicon, GSSI and the team of IYAFA (Selection committee).
When selecting applications, the call promoters may request additional documentation or interviews both for the purpose of verifying compliance with eligibility requirements and to facilitate proposal evaluation.
Camera recipients:
Participants to the Storytelling Lab who will be given a GoPro camera will be selected based on:
The evaluation will be carried out by a team of 4 judges from The Lexicon, GSSI and the team of IYAFA (Selection committee).
Incidental expenses and all other costs and expenses which are not specifically listed in these Official Rules but which may be associated with the acceptance, receipt and use of the Storytelling Lab and the camera are solely the responsibility of the respective participants and are not covered by The Lexicon or any of the A Greener Blue partners.
All participants who receive a Camera are required to sign an agreement allowing GoPro for a Cause, The Lexicon and GSSI to utilize the films for A Greener Blue and their promotional purposes. All participants will be required to an agreement to upload their footage into the shared drive of The Lexicon and make the stories, films and images available for The Lexicon and the promoting partners of A Greener Blue.